1516 Legacy Cir, Naperville, IL 60563
What Causes Periodontal Disease
What is Periodontal Disease?
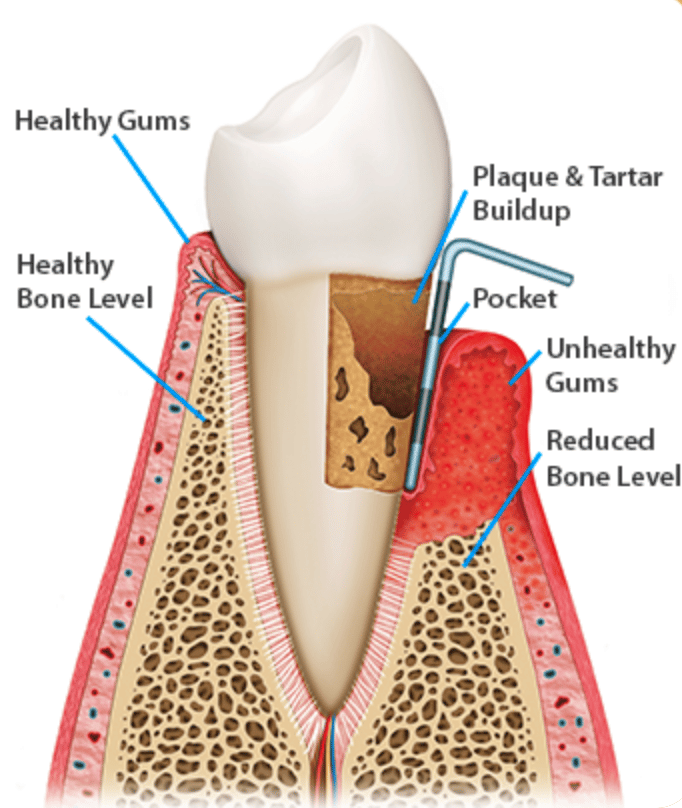
Periodontal Disease, also known as gum disease or periodontitis, is an inflammatory disease associated with bone loss and tissue damage in the mouth. Periodontal disease starts as gingivitis, which is inflammation of the gum tissue caused by plaque and bacteria. This is usually caused by poor brushing and flossing habits at home. The plaque contains harmful bacteria, and when left on the gum tissue it promotes inflammation. This causes tender gums and bleeding. Gingivitis can be reversed with professional dental cleanings and pristine oral hygiene habits at home.
When the bacteria is removed and the gums can heal, they can return to a state of health. In patients with gingivitis who let their condition worsen, periodontal disease can occur. Once the attachment levels start to decline, it is no longer reversible and is then classified as periodontitis. Attachment levels can be described as the components holding your tooth in your mouth; this includes bone and gum tissue. When gum tissue is lost it is classified as recession. This can be seen visually by patients because it involves exposure of the tooth root. This can cause some sensitivity because the root of the tooth is typically covered by gum tissue and is not meant to be exposed.
Periodontal Symptoms?
Some patients may not even be aware that they have this condition until their hygienist or dentist brings it to their attention. Periodontal disease typically is not painful to patients during everyday life. This one of the main reasons periodontal disease often goes unnoticed by patients for many years. It can be detected at a routine cleaning, which is why it is so important to stay on top of regular dental appointments. Some periodontal symptoms may include sore and bleeding gums, recession, spaces between the teeth, loose teeth, and calculus, more commonly known as tartar, buildup on teeth.
Periodontitis can be identified on x-rays because dentists and hygienists are able to see the bone levels. Sometimes tartar below the gum-line can also show up on x-rays as well. Hygienists can also identify areas of attachment loss and inflammation by using a periodontal probe. This tool is used to take measurements of bone levels and recession. Measurements ranging from 1-3 mm are in the healthy range; anything 4 or above is a concern that should be brought to the patient’s attention. Areas that bleed upon probing are also recorded. Active periodontal disease involves bleeding, whereas periodontitis in a maintenance phase will have bone loss, but not bleeding present.
What Are The Causes of Periodontal Disease?
Various causes of periodontitis include poor oral hygiene habits at home, infrequent dental cleanings, and having a compromised immune system. Poor oral hygiene will lead to plaque, calculus, and stain build up on the teeth. The plaque and calculus both harbor a significant amount of bacteria; this bacteria irritates the gum tissue and causes inflammation. The stain on the teeth, although it does not contain bacteria, it creates a rough surface on the teeth. The rough surfaces invite plaque to stick onto the teeth and harden into calculus.
Infrequent dental cleanings will lead to periodontal disease because once the plaque mineralizes and hardens into calculus, it cannot be removed at home. Calculus can only be removed from the tooth surface with special instruments that a dental hygienist is trained to use. Also, patients with compromised immune systems are not able to fight the bacteria in their mouth as well as someone with optimal health. Even with good oral habits, some patients may be more susceptible to periodontal disease than others.
Risk Factors of Periodontal Disease
Some risk factors for periodontitis include pre-existing gingivitis, smoking, medications that cause dry mouth, type II diabetes, pregnancy, and having health conditions that are associated with weakened immune systems. As discussed previously, gingivitis is the first stage of gum disease. Patients who do not take the steps to reverse gingivitis are more susceptible to periodontal disease because they are one step away from being in the next category.
Patients who smoke are also more apt to develop periodontal disease. Nicotine, which is found in both traditional cigarettes and e-cigarettes, is a vasconscitior. This means that the blood flow, which promotes healing, is restricted from the gum tissue. Smoking also decreases saliva flow, which can be very detrimental to a patient’s oral health. Saliva has many roles in keeping the mouth healthy including: preventing tooth decay, limiting bacterial growth, washing away food, and aiding in speech and swallowing. Dry mouth is also a side effect of some medications.
Patients taking medications that cause dry mouth are at risk for periodontal disease because saliva rinses food and bacteria off your teeth throughout the day. Without enough saliva, patients are more at risk. Type II diabetes are another group with a higher probability of acquiring periodontal disease , especially if their diabetes is not well controlled. Diabetic patients are more susceptible to infections, periodontitis included. It is also true that these two conditions go hand and hand.
Periodontal disease can actually worsen the effects that diabetes has on the body. Untreated periodontal disease, along with other bacterial infections, can cause blood sugar levels to rise. Pregnant patients are also at risk because gum tissues are usually more inflamed during pregnancy. This is commonly referred to as “pregnancy gingivitis.” If not properly maintained, pregnant women are more likely to develop periodontal disease. As previously mentioned, weakened immune systems interfere with the body’s ability to fight bacteria in the mouth. Patients with these, and many other risk factors, need to stay on top of their oral health even more than usual.
Although it cannot be cured, periodontal disease can be treated in a variety of ways including surgical and nonsurgical procedures. It is best to treat periodontitis as early as possible. Once periodontitis has been initially treated, it is important to maintain the gum health by continuing to come for regular appointments with your hygienist so it can be monitored. Your dentist and hygienist will work together to create a plan for your individual needs. Call our office to schedule an appointment today!