1516 Legacy Cir, Naperville, IL 60563
TMJ Surgery: Why You Should Consider It?

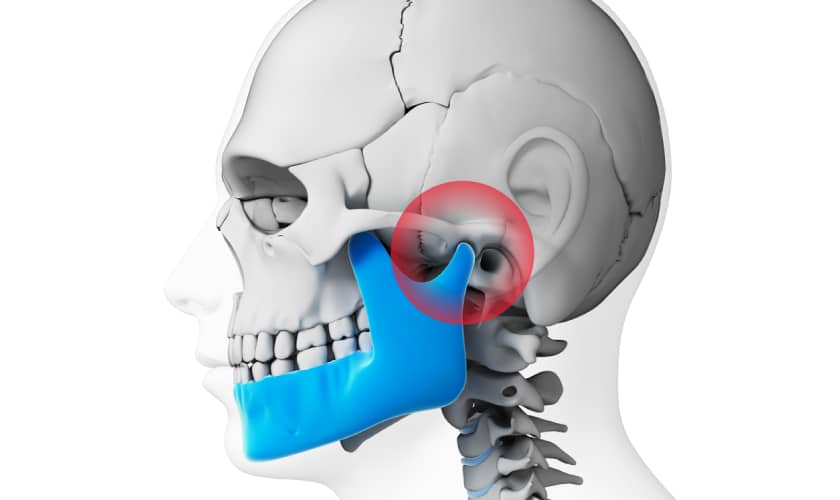
The temporomandibular joint (TMJ) is an intricate part of your body, responsible for the seamless movement of your jaw. However, for some individuals, TMJ disorders can lead to persistent pain, discomfort, and limitations in daily life. While various treatments are available, including non-surgical options, TMJ surgery becomes a consideration in some cases. In this comprehensive guide, we will explore the intricacies of TMJ surgery, discussing when it might be the right option, the types of surgeries available, potential risks, and alternative treatments. We aim to provide valuable insights to help you decide about your TMJ disorder management.
What Are TMJ Disorders?
TMJ disorders encompass a range of conditions that affect the temporomandibular joint and the surrounding muscles. Common symptoms include jaw pain, headaches, clicking or popping sounds when you chew or speak, and limited jaw movement. These issues can result from various factors, including stress, teeth grinding, misaligned teeth, or injury. In many cases, TMJ disorders can be managed with conservative treatments like lifestyle modifications, physical therapy, medications, and dental appliances. However, for some individuals, these methods may not provide sufficient relief, and that’s when the consideration of TMJ surgery arises.
When is TMJ Surgery Considered?
TMJ surgery is typically considered when conservative treatments have been exhausted and the patient continues to experience severe pain and dysfunction in their jaw. It’s crucial to explore surgery only after a thorough evaluation by a qualified healthcare professional, as surgery carries inherent risks and should not be the first option. Here are some scenarios when TMJ surgery might be considered:
- Structural Issues: If there are structural problems in the jaw joint, such as damage to the joint or surrounding tissues, surgery may be necessary to repair or replace damaged components.
- Failed Conservative Treatments: When non-surgical approaches like physical therapy, medications, and lifestyle changes have not provided relief, surgery may become a viable option.
- Disc Displacement: Surgical repositioning or disc replacement may be recommended if the articular disc within the TMJ is significantly displaced and causing severe pain and dysfunction.
- Severe Degeneration: Surgery may be necessary to address the joint’s deterioration in cases of advanced joint degeneration or osteoarthritis.
- Traumatic Injury: If the TMJ has suffered a traumatic injury, such as a fracture, surgery may be required to restore function and alleviate pain.
It’s crucial to thoroughly evaluate and consult with an oral and maxillofacial dentist or a specialist in TMJ disorders to determine if surgery is the right course of action for your specific condition.
Types of TMJ Surgery
Several surgical procedures can address TMJ disorders, each tailored to the individual’s unique situation. The choice of surgery depends on the underlying issue and its severity. Here are some common types of TMJ surgery:
- Arthroscopy: In this minimally invasive procedure, a small camera (arthroscope) is inserted into the joint to assess and treat the problem. It is often used for diagnosing and treating mild to moderate TMJ issues.
- Arthrocentesis: This procedure involves flushing the joint with sterile fluids to remove debris and inflammatory byproducts. It can help reduce pain and improve joint function.
- Open-Joint Surgery: Open-joint surgery may be necessary for more complex cases. This involves making an incision to access the joint directly. It can be used for repairing or replacing damaged joint components.
- Total Joint Replacement: In severe cases of TMJ degeneration, total joint replacement may be considered. This surgery involves replacing the entire joint with an artificial prosthesis.
- Repositioning Surgery: If the TMJ disc is displaced, surgical repositioning may be performed to correct its alignment within the joint.
- Orthognathic Surgery: In cases where the TMJ disorder is associated with jaw misalignment, orthognathic surgery may be recommended to reposition the jaw, improving joint function and alignment.
Discussing the specific surgical options with your healthcare provider and understanding the potential benefits and risks associated with each procedure is crucial. Your treatment plan should be tailored to your unique condition and needs.
Lifestyle Modifications after TMJ Surgery
Temporomandibular Joint (TMJ) surgery can be life-changing for individuals suffering from severe jaw joint problems. After undergoing this surgery, it’s essential to make specific lifestyle modifications to ensure a smooth recovery and maintain long-term oral health.
Soft Diet Transition
After TMJ surgery, you’ll need to modify your diet temporarily. Initially, focus on consuming soft foods that require minimal chewing, such as yogurt, mashed potatoes, and smoothies. Avoid hard, crunchy, or chewy foods that could strain your healing jaw joint. As you recover, your dentist will guide you on gradually reintroducing a regular diet.
Pain Management
Expect some discomfort following TMJ surgery. Your dentist will prescribe pain medications to help manage the pain. It’s essential to follow the recommended dosage and not skip any doses. Additionally, applying ice packs to the surgical area as directed can reduce swelling and discomfort.
Oral Hygiene
Maintaining proper oral hygiene is crucial after TMJ surgery. Gentle brushing and flossing are essential but do not irritate the surgical site. Your dentist may recommend a special mouthwash or oral rinse to keep your mouth clean without causing harm to the healing tissues.
Avoiding Excessive Jaw Movement
To promote healing, it’s essential to limit excessive jaw movement. Avoid activities that involve wide mouth opening, such as yawning, singing, or excessive talking. Your dentist will provide guidelines on protecting your jaw during daily activities.
Physical Rest
Adequate rest is essential for a swift recovery. Avoid strenuous physical activities, especially in the initial days following surgery. Resting allows your body to divert energy toward healing and minimizes the risk of complications.
Follow-up Appointments
Keep all your scheduled follow-up appointments with your dentist. These visits are crucial for monitoring your progress and promptly addressing any concerns or complications. Your dentist will guide you on when it’s safe to resume regular activities.
Stress Management
Stress can exacerbate jaw problems. Consider incorporating stress management techniques, such as meditation, deep breathing exercises, or yoga, into your daily routine. Reduced stress levels can contribute to a smoother recovery.
Avoiding Harmful Habits
If you have habits like teeth grinding or clenching, addressing them after TMJ surgery is essential. These habits can strain the jaw joint and hinder your recovery. Your dentist may recommend a mouthguard or other strategies to break these habits.
Hydration and Nutrition
Staying hydrated is essential for overall well-being and healing. Ensure you’re drinking enough water throughout the day. Maintaining a balanced diet rich in vitamins and minerals can also support the healing process.
Patience and Positivity
Finally, maintain a positive attitude and be patient with your recovery. TMJ surgery is a significant step toward better oral health, but it may take time to see the full benefits. Stay committed to your post-surgery care plan, and don’t hesitate to communicate any concerns with your healthcare provider.
TMJ surgery is a significant decision that should be made after careful consideration and consultation with healthcare professionals. While it can offer relief to those suffering from severe TMJ disorders, exploring non-surgical options and alternative treatments is essential first. The choice of surgery should be based on the specific diagnosis, the severity of symptoms, and the potential benefits and risks.
Remember that every individual’s situation is unique, and no one-size-fits-all solution exists. Working closely with your healthcare team to develop a tailored treatment plan that addresses your specific needs and goals is crucial.
Whether you ultimately choose surgery or opt for alternative treatments, the primary goal is to alleviate your TMJ-related pain and improve your quality of life. You can find relief and regain control over your oral health and overall well-being with the right approach and guidance.
FAQs
Q: How long does the recovery period after TMJ surgery usually last?
A: The recovery period can vary depending on the type of TMJ surgery and your healing process. It may take several weeks to a few months to fully recover. During this time, you’ll need to follow your dentist’s post-operative instructions and attend follow-up appointments to monitor your progress.
Q: Is TMJ surgery a permanent solution to my jaw problems?
A: TMJ surgery can provide long-term relief for many individuals, but it’s not always a permanent solution. Success depends on various factors, including the surgery type, adherence to post-operative care instructions, and lifestyle habits. In some cases, additional treatments or adjustments may be necessary in the future to maintain optimal jaw health.
Q: What can I do to manage pain and discomfort after TMJ surgery?
A: Post-surgery discomfort involves following your dentist’s prescribed pain management plan. This typically includes pain medications and the application of ice packs to reduce swelling. Adequate rest, stress management techniques, and avoiding activities that strain the jaw joint are also essential for a smoother recovery.
Q: Are there alternative treatments for TMJ disorders besides surgery?
A: Yes, before considering surgery, it’s advisable to explore non-surgical treatments. These include physical therapy, lifestyle modifications, medications, and dental appliances like splints or mouthguards. Consult a TMJ specialist to determine the most appropriate approach for your condition.