1516 Legacy Cir, Naperville, IL 60563
How to Treat Periodontal Disease (Gum Disease)
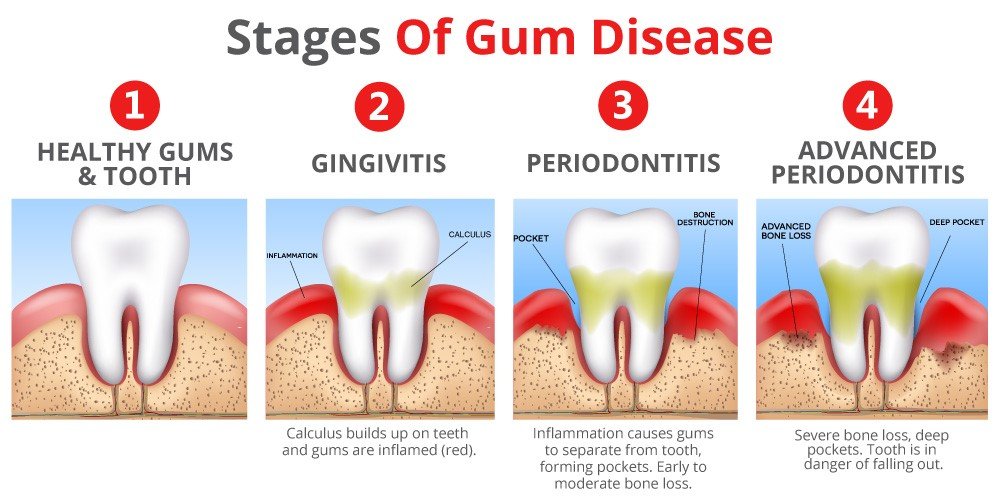
Don’t ignore bleeding gums, persistent bad breath, or gums that appear to be receding from your teeth. These are potential early indicators of periodontal disease. If left untreated, gum disease may result in tooth loss and can negatively impact your overall health.
Fortunately, there is treatment for periodontal disease, particularly in its early stages. With appropriate interventions like scaling and root planing, you can prevent further progression of disease and maintain your smile.
In this guide, our dental experts explain common signs you may have periodontal disease, how to treat periodontal disease, and when you should see a dentist.
Common Signs You May Have Periodontal Disease
Gum disease begins quietly and is often unrecognized. Additionally, most people don’t notice it until the condition becomes more advanced. Recognizing the early symptoms can significantly improve treatment outcomes.
You might be suffering from periodontal disease if you’ve noticed any of the following::
- Gums that bleed easily while brushing or flossing
- Red, swollen, or tender gums
- Chronic bad breath or a bad taste in the mouth
- Receding gums that make teeth look longer
- Loose or shifting teeth
- Pain or discomfort while chewing
- Pus between the gums and teeth
- Changes in your bite or tooth alignment
How to Treat Periodontal Disease?
Dentists treat periodontitis with surgical or nonsurgical methods, depending on how advanced the damage is. Dentists and hygienists will help guide patients towards the best options for how to treat periodontitis.
Dental Cleanings
The nonsurgical method of treating periodontal disease begins with professional dental cleaning. One of these is:
Scaling and Root Planing
Dental professionals often refer to scaling and root planing as a “deep cleaning,” and it is the first line of treatment for patients with active periodontal disease.
This process removes plaque, calculus, and bacteria from the gum pockets and along the roots of the teeth. It is a more extensive process than the usual dental cleaning, and it may be necessary to do multiple procedures.
To keep the patient comfortable and allow for a thorough cleaning, dentists routinely use local anesthesia. They may administer it using small injections or apply a numbing gel to the gums.
After treatment, they typically schedule cleanings every three months because patients can’t manage the depth of the periodontal pockets with home care alone.
Surgical treatment for advanced periodontitis
For more severe cases, periodontal surgery may be necessary. Patients who require surgery are referred to a periodontist.
Bone Grafting
Periodontal bone disease may require bone grafting. The grafting material may come from the patient, a donor, or a synthetic source.
Gum Grafting
Gum grafting treats gum recession by covering exposed tooth roots. Dentists usually take the graft tissue from the roof of the patient’s mouth or use tissue from a donor source.
Flap Surgery
Flap surgery involves gently lifting the gums to remove deep tartar and bacteria. After cleaning the roots, the dentist repositions the gum tissue snugly around the teeth to reduce pocket depth.
In some cases, they performs guided tissue regeneration along with flap surgery by placing a mesh barrier to encourage proper regrowth of bone and gum tissue.
Bone Surgery
Bone surgery reshapes damaged bone to eliminate areas where bacteria can easily accumulate. Dentists often perform this procedure after flap surgery.
Frequently Asked Questions
Periodontitis is primarily caused by poor oral hygiene. Other contributing factors include smoking, genetics, diabetes, hormonal changes, certain medications, and infrequent dental visits.
Early symptoms may include bleeding gums, redness or swelling, persistent bad breath, gum recession, and sensitivity. Many patients do not experience pain in the early stages.
Dentists keep scaling and root planing comfortable by numbing the area with local anesthesia or a numbing gel. Some mild soreness may occur afterward but usually resolves quickly.
Not all patients need surgery. Dentists typically recommend surgery only for advanced cases when deep pockets and bone loss cannot be managed with nonsurgical treatment alone.
No. Dentists use antibiotics alongside professional cleanings, not as a standalone treatment. They help reduce bacteria but cannot remove plaque or tartar.
If left untreated, periodontitis can cause tooth loss, progressive bone damage, and ongoing gum infections. It has also been linked to systemic health conditions, including heart disease and diabetes.
Home care alone cannot treat periodontitis, but it is essential for managing it. Brushing twice daily, flossing, using a water flosser, and following professional recommendations are critical.
Yes. Electric toothbrushes are highly effective for periodontal patients because they remove plaque more efficiently than manual toothbrushes.
Yes. Research shows a connection between periodontal disease and conditions such as diabetes, heart disease, and respiratory issues.
You should see a dentist if you notice bleeding gums, persistent bad breath, loose teeth, gum recession, or discomfort while chewing.